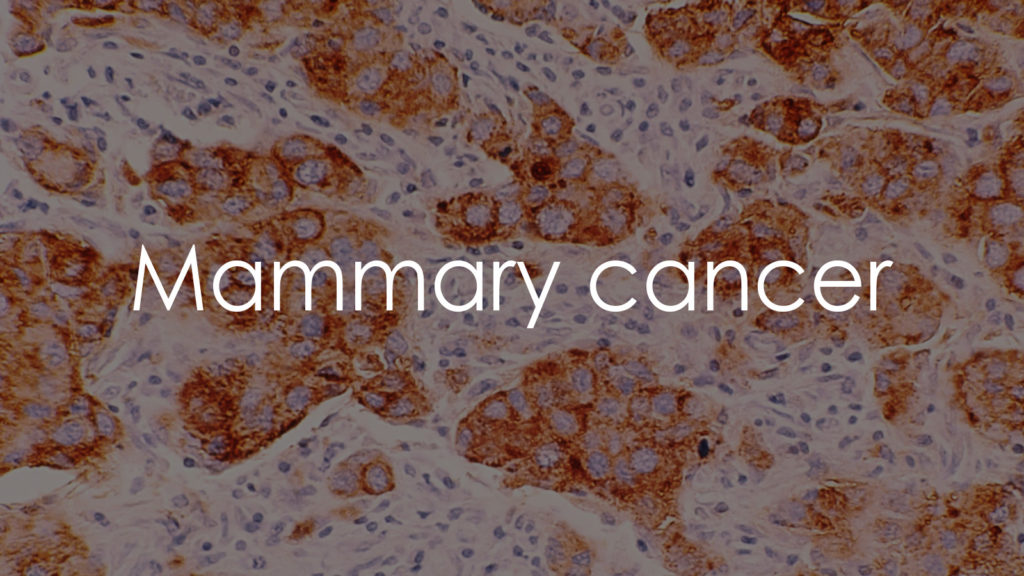
Mammary cancer, more commonly referred to as breast cancer, is a type of cancer that forms in the cells of the breasts, a condition predominantly affecting women, though it can also occur in men. It’s one of the most common cancers diagnosed in women worldwide. Breast cancer can arise in different parts of the breast, such as the ducts (ductal carcinomas) that carry milk to the nipple or the glands (lobular carcinomas) that produce milk. The prognosis and treatment depend on the cancer type, stage, and other factors. Early detection through screening can significantly improve outcomes, making awareness and regular examinations critical.
Causes
The exact cause of mammary cancer is not fully understood, but several risk factors have been identified that may increase the likelihood of developing the disease:
- Gender: Being a woman is the main risk factor for developing breast cancer.
- Age: The risk increases with age, with most breast cancers diagnosed in women over 50.
- Genetic Mutations: Inherited mutations in genes such as BRCA1 and BRCA2 significantly increase the risk.
- Family History: Having a close relative with breast cancer increases one’s risk.
- Personal History: Women who have had breast cancer before are more likely to have it again.
- Radiation Exposure: Previous radiation treatments to the chest area increase the risk.
- Hormonal Factors: Early menstruation, late menopause, having children late or not at all, and hormone therapy after menopause can increase risk.
- Lifestyle Factors: Being overweight, physically inactive, consuming alcohol excessively, and certain dietary habits can contribute to breast cancer risk.
Symptoms
Symptoms of mammary cancer can vary from person to person but may include:
- A Lump or Thickening in the Breast: The most common symptom, often discovered by breast self-exam or mammography.
- Changes to the Skin: Such as dimpling, puckering, redness, or scaling.
- Changes to the Nipple: Including inversion, discharge not related to breastfeeding, or flaking of the nipple skin.
- A Change in Breast Size or Shape: Noticeable over a short period.
- Pain: In the breast or armpit not related to the menstrual cycle.
- Swelling: In all or part of the breast, even if no lump is felt.
Not all lumps or changes in the breast indicate cancer, but they should prompt a visit to a healthcare provider for evaluation. Early detection and treatment are crucial in managing mammary cancer effectively and improving the prognosis.
Diagnostics
Diagnosing mammary (breast) cancer involves a combination of physical examinations, imaging tests, and biopsies to determine the presence and extent of cancer. Key diagnostic steps include:
- Breast Examination: Both self-exams by the patient and clinical exams by healthcare providers can help identify any lumps or changes in the breast.
- Mammography: An X-ray of the breast is the most common screening tool for breast cancer. It can detect tumors that are too small to be felt and can also identify suspicious areas that may require further testing.
- Ultrasound: Uses sound waves to produce images of structures within the breast. It can help distinguish between solid masses (potentially cancerous tumors) and fluid-filled cysts.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the breast and is particularly useful in women with a high risk of breast cancer or dense breast tissue.
- Biopsy: The definitive way to diagnose breast cancer, involving the removal of a small amount of tissue for examination under a microscope. There are several biopsy techniques, including fine-needle aspiration, core needle biopsy, and surgical biopsy.
- Molecular Testing of the Tumor: To identify specific genes, proteins, and other factors unique to the tumor. This information can help guide treatment decisions.
Treatment
Treatment for mammary cancer varies depending on the cancer’s stage, type, and other individual factors, including the patient’s overall health and preferences. Common treatment options include:
- Surgery:
- Lumpectomy: Removal of the tumor and a small margin of surrounding tissue, preserving most of the breast.
- Mastectomy: Removal of one or both breasts, partially (segmental mastectomy) or completely (total mastectomy).
- Radiation Therapy: Uses high-energy waves to target and kill cancer cells. Often used after surgery to eliminate any remaining cancer cells in the breast, chest wall, or axilla (underarm area).
- Chemotherapy: Involves the use of drugs to kill cancer cells, typically used when the cancer is considered aggressive, has spread beyond the breast and lymph nodes, or to reduce the size of the tumor before surgery (neoadjuvant chemotherapy).
- Hormone Therapy: For cancers that are hormone receptor-positive, medications can help block the body’s natural hormones (estrogen and progesterone) from supporting the growth of cancer cells.
- Targeted Therapy: Targets specific characteristics of cancer cells, such as a protein that allows the cancer cells to grow in a rapid or abnormal way. Examples include HER2-targeted therapies for cancers that overexpress the HER2 protein.
- Immunotherapy: Utilizes the body’s immune system to fight the cancer, for cancers that are found to be susceptible to this approach.
- Bone-directed Therapy: For patients whose cancer has spread to the bone, these treatments help protect the bones against the effects of cancer.
Prevention
While not all cases of breast cancer can be prevented, there are strategies that can help reduce the risk and detect it early:
- Regular Screening: Mammograms and breast exams can help detect breast cancer early when it is most treatable.
- Healthy Lifestyle: Maintaining a healthy weight, eating a balanced diet rich in fruits and vegetables, engaging in regular physical activity, and limiting alcohol consumption can reduce breast cancer risk.
- Avoid Smoking: There’s growing evidence that smoking is linked to a higher risk of breast cancer, especially in premenopausal women.
- Limit Exposure to Radiation and Environmental Pollution: Minimize exposure to radiations, such as those from medical-imaging methods, and avoid environmental pollutants when possible.
- Breast-feeding: Breast-feeding for several months can also reduce the risk of breast cancer. The longer you breast-feed, the greater the protective effect.
- Hormone Therapy Consideration: Women should talk with their healthcare providers about the risks and benefits of hormone replacement therapy if considering it for menopause symptoms.
Complications
Breast cancer can lead to several complications, especially if not detected or treated early:
- Metastasis: Breast cancer can spread to other parts of the body, such as the bones, liver, lungs, or brain, leading to more severe health issues.
- Lymphedema: Swelling in the arm or hand (lymphedema) can occur after surgery or radiation therapy that involves the lymph nodes.
- Side Effects of Treatment: Chemotherapy, radiation therapy, and hormonal therapy can have significant side effects, including fatigue, menopausal symptoms, and increased risk of other cancers.
- Psychological Impact: The diagnosis and treatment of breast cancer can have a significant emotional and psychological impact, leading to anxiety, depression, and changes in body image.
Conclusion
Mammary (breast) cancer is a complex disease with significant implications for women’s health worldwide. Advances in understanding, prevention, screening, and treatment have improved survival rates and quality of life for many affected women. Adoption of a healthy lifestyle, combined with regular screening and awareness of risk factors, plays a crucial role in prevention and early detection. For those diagnosed with breast cancer, a multidisciplinary approach to treatment tailored to the individual’s specific situation can effectively manage the disease. Ongoing research and support for those affected by breast cancer are essential to continue improving outcomes and providing hope to patients and their families.