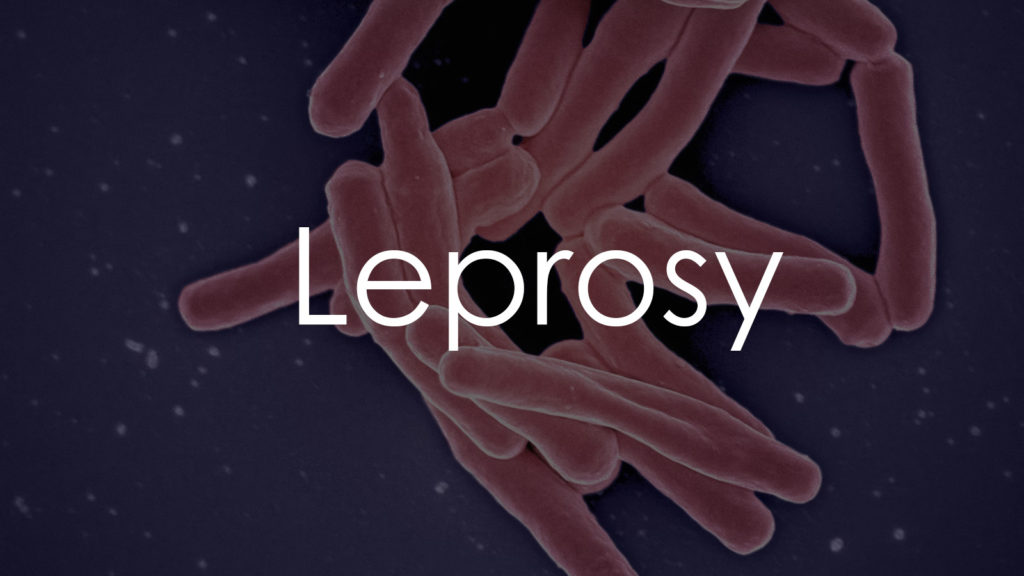
Leprosy, a chronic infectious disease caused by the bacterium Mycobacterium leprae, has a rich historical context. Once a source of immense social stigma and widespread fear, leprosy remains a health concern in various parts of the world. This article delves into the causes, symptoms, diagnosis, treatment, and prevention of leprosy, aiming to provide a comprehensive understanding of the disease in its current global context.
Causes
Leprosy, a disease as ancient as it is complex, is primarily caused by the bacterium Mycobacterium leprae. This section delves into the intricate details of how this chronic infectious disease is transmitted and the various factors that contribute to its development. Understanding the causes of leprosy is crucial for effective prevention strategies and provides insight into why certain populations are more affected than others.
- Mycobacterium leprae: The primary causative agent of leprosy, this bacterium is slow-growing and mainly affects the skin and nerves.
- Transmission: Leprosy is believed to be transmitted through prolonged close contact with untreated, infected individuals. It is often spread via respiratory droplets, although the exact mechanism is not fully understood.
- Genetic Factors: Some individuals are genetically more susceptible to leprosy. This susceptibility is thought to be linked to the way an individual’s immune system responds to the Mycobacterium leprae.
- Environmental Influence: Overcrowded living conditions, poor sanitation, and other environmental factors can increase the risk of transmission. These conditions are more prevalent in certain regions, particularly in parts of Africa, Asia, and Latin America.
- Immune System Response: The body’s immune response plays a significant role in the development of the disease. Those with a weaker immune response are more likely to develop more severe forms of leprosy.
Symptoms
The symptoms of leprosy are diverse and often present a diagnostic challenge. In this section, we explore the range of clinical manifestations of leprosy, from early signs to more advanced stages. Recognizing these symptoms is vital for early detection and timely treatment, which can significantly reduce the risk of long-term complications.
- Skin Lesions: Painless skin lesions that are lighter than the normal skin tone are one of the earliest signs. These lesions may also have decreased sensation to touch, heat, or pain.
- Nerve Damage: Numbness and muscle weakness, particularly in the hands, feet, and limbs, can occur due to nerve damage caused by the bacterial infection.
- Muscular Weakness: Progressive muscle weakness and paralysis, especially of the small muscles of the hand, can occur in advanced cases.
- Eye Problems: Chronic infection can lead to eye problems, including dryness and reduced blinking, which can result in blindness if not treated promptly.
- Nasal Congestion: Some patients experience chronic nasal congestion and nosebleeds due to mucosal involvement.
- Systemic Symptoms: In more severe cases, systemic symptoms like fatigue, weight loss, and fever may be present.
Types
Leprosy is classified into two main types based on the severity and number of bacteria present:
- Paucibacillary Leprosy: Characterized by fewer lesions and less bacterial load.
- Multibacillary Leprosy: Involves more widespread disease with numerous lesions and a higher bacterial load.
Understanding the causes and recognizing the symptoms of leprosy are key to early diagnosis and treatment, which can prevent disability and stop the transmission of the disease. Despite its historical stigma, leprosy is now a treatable condition with a good prognosis when detected early. Public health efforts, improved living conditions, and ongoing research are critical in the global fight against leprosy.
Diagnostics
Diagnosing leprosy involves a combination of clinical evaluation and diagnostic tests. This section outlines the various methods used to diagnose leprosy, including skin biopsies, nerve function tests, and advanced molecular techniques. Early and accurate diagnosis is key to effective management and prevention of disease transmission.
- Clinical Examination: The first step in diagnosing leprosy involves a thorough clinical examination. Doctors look for characteristic skin lesions that are lighter than the normal skin tone and may have reduced sensation to touch, temperature, or pain.
- Skin Smear Test: This test involves taking a sample from the affected skin area and staining it for the presence of Mycobacterium leprae. However, its sensitivity varies, especially in paucibacillary (fewer bacteria) cases.
- Skin Biopsy: A biopsy provides more definitive information. It involves examining a small piece of skin tissue under a microscope to identify the presence of leprosy bacilli.
- Nerve Function Tests: Since leprosy affects nerve function, tests to assess the loss of sensation or muscle weakness can be indicative.
- Polymerase Chain Reaction (PCR): PCR tests for leprosy are becoming more common. They can detect the DNA of Mycobacterium leprae from skin samples, offering a more accurate and quicker diagnosis.
- Serological Tests: These tests detect antibodies against Mycobacterium leprae, but they cannot distinguish between past exposure and active infection.
Treatment
The treatment of leprosy has evolved significantly over the years, turning a once-feared disease into a manageable condition. This section covers the current treatment protocols, including the use of multidrug therapy (MDT) and supportive care measures. It also highlights the importance of completing the treatment regimen and addresses the challenges in managing and preventing leprosy-related disabilities.
- Multidrug Therapy (MDT): The World Health Organization (WHO) recommends a multidrug therapy for leprosy, which has proven to be highly effective. This therapy typically includes a combination of dapsone, rifampicin, and clofazimine.
- Paucibacillary Leprosy: The MDT for this form typically lasts for 6 months.
- Multibacillary Leprosy: Treatment for this form is more intensive and usually lasts for 12 months or longer.
- Monitoring and Side Effects: Regular monitoring during treatment is essential to check for any side effects of the drugs and to ensure that the treatment is effective.
- Prevention of Disability: Alongside MDT, treatment focuses on preventing disability and managing complications. This includes physiotherapy and occupational therapy to maintain muscle strength and prevent contractures.
- Eye Care: As leprosy can affect the eyes, regular ophthalmological examinations are important to prevent blindness.
- Patient Education and Support: Educating patients about their condition, treatment regimen, and the importance of completing the full course of MDT is essential. Additionally, psychological and social support plays a key role in holistic care.
Conclusion
Leprosy, although significantly controlled and treated in many parts of the world, still requires attention and awareness. Understanding its causes, symptoms, and treatment options is crucial for effective management and prevention. Equally important is the destigmatization of leprosy, ensuring that those affected receive not only medical care but also social support and acceptance. Continued efforts in public health, research, and education are vital in the global fight against leprosy.